“I’m just tired” — how often have you said that to explain away a foggy brain, low energy, or even a missing spark in the bedroom? You might treat sleep as optional, giving it up for extra work, late-night scrolling, or one more episode.
But there are questions you should be asking yourselves: What if not getting enough sleep does more than just make you feel tired? What if it quietly affects your sexual health and makes it harder to get or keep an erection?
Erectile dysfunction, or ED, is more common than most people realize. It’s usually blamed on stress, age, or health problems like diabetes or heart disease, but there’s one cause that often gets overlooked — lack of sleep.
New research shows that poor sleep interferes with hormones, blood flow, and many other systems that keep your sexual life healthy.
So before reaching for quick fixes or ED pills, it’s worth taking a closer look at how well you’re actually sleeping.
In this blog, you’ll discover:
- Can poor sleep cause erectile dysfunction?
- Why does sleep matter for men’s health?
- Key Sleep problems linked to ED
- Ways to improve your sleep and boost your intimate life
Why Sleep is More Important to Men’s Health Than You Might Think
We often hear that diet and exercise are the pillars of good health. But here’s something many don’t realize: sleep is just as important, especially when it comes to men’s health.
It’s not only about feeling rested the next day, it’s more than that!
Sleep plays a huge role in how your body functions overall, including your heart, hormones, and yes, sexual health.
Among many sexual health conditions, ED is one of the most common conditions where a man struggles to get or keep an erection. Experts estimate that by 2025, around 300 million men worldwide will be affected by ED. Beyond the physical challenge, it can take a big toll on self-esteem and relationships.
What’s becoming clear through research and leading health organizations, like the American Heart Association, is that sleep affects many factors related to ED. Poor sleep can lead to issues with blood pressure, cholesterol, and body weight, all of which are important for cardiovascular health and are closely linked to erectile function.
This means sleep doesn’t just influence ED directly. It also affects it indirectly by impacting overall health.
This isn’t just a myth; sleep deprivation and erectile dysfunction are scientifically linked. Let’s take a closer look at the research that supports this.
Sleep Deprivation and Erectile Dysfunction: What the Research Shows
Let’s get into what the research really says. The connection between sleep and erectile dysfunction isn’t just a theory — it’s backed by solid science.
Multiple studies confirm that poor sleep quality and sleep disorders significantly raise the risk of ED. For instance, a 2009 study published in the Journal of Sexual Medicine found that 69% of men with Obstructive Sleep Apnea (OSA) also had ED. Another study from 2016 echoed this, showing a 63% ED rate in men with OSA, much higher than the 47% in those without the condition.
Sleep apnea isn’t the only concern, & It doesn’t stop there
In a survey of men with ED, 55% showed signs of sleep apnea, indicating many cases could be linked to undiagnosed sleep issues. And it’s not just about diagnosed disorders—poor sleep quality alone has a big impact. A study across 12 clinics found that 44.5% of men with erection issues also had poor sleep, based on standardized sleep assessments.
Even young men are affected.
A survey of young university students aged 18–30 found that over half reported poor sleep. Among them, nearly 73% had mild ED, and those with poor sleep were over six times more likely to experience erectile issues, even after accounting for age and health.
So, what does this all mean?
The evidence is clear: sleep problems are not just side effects—they’re often key contributors to ED.
Here’s a quick summary of the research:
| Prevalence of ED in Common Sleep Disorders | |
| Sleep Disorder / Condition | Reported ED Prevalence / Association |
| Obstructive Sleep Apnea (OSA) | 63% – 80% of men with OSA also experience ED; 9.44 times higher risk compared to men without OSA |
| Insomnia | Men with untreated insomnia are more likely to report ED |
| Restless Leg Syndrome (RLS) | Men with RLS are more likely to experience ED due to sleep fragmentation and poor sleep quality |
| Poor Sleep Quality (General) | 44.5% of men with ED report poor sleep; young men with poor sleep have a 6.48 times higher risk of ED |
All signs point to one clear conclusion:
If you’re facing erectile dysfunction, don’t overlook your sleep. It might just be the missing piece.
How Sleep Loss Disrupts Erections? The Key Mechanisms Explained
We often treat sleep as optional. But when it comes to sexual health, especially erectile function, sleep is essential. Here’s how a lack of quality sleep can quietly sabotage your performance in bed.
-
Hormonal Disruption
Testosterone is the key male hormone responsible for libido and erections. Most of it is produced during deep sleep, especially in Rapid Eye Movement (REM) stages. When sleep is short or disturbed, testosterone production drops. Even one week of poor sleep can lower levels by up to 15%, which directly impacts sexual desire and performance.
-
Reduced Blood Flow
Erections rely heavily on good blood circulation. Poor sleep raises blood pressure, triggers inflammation, and damages blood vessels. It also reduces nitric oxide, a molecule needed to help blood vessels relax. The result is reduced blood flow to the male genital organ, making it harder to get or maintain an erection.
-
Nerve System Disruption
Your brain and nerves coordinate the erection process. Sleep deprivation activates stress hormones like cortisol and adrenaline, which throw off this balance. The nervous system stays in a “fight-or-flight” mode, working against the relaxation needed for arousal.
-
Weight and Metabolic Changes
When you’re sleep-deprived, hormones like ghrelin and leptin go out of sync. This increases appetite, especially for high-calorie foods, and contributes to weight gain. Obesity is closely linked to erectile dysfunction and also worsens sleep quality, creating a vicious cycle.
-
Inflammation and Oxidative Stress
Chronic poor sleep raises levels of inflammation in the body. This damages blood vessels and further impairs the flow of oxygen and nutrients needed for sexual function. Oxidative stress also reduces nitric oxide, compounding the problem.
-
Mental Health Strain
Anxiety, depression, and irritability often follow sleep deprivation. These emotional issues are deeply connected to ED. In fact, stress from ED itself can worsen sleep, creating a frustrating feedback loop.
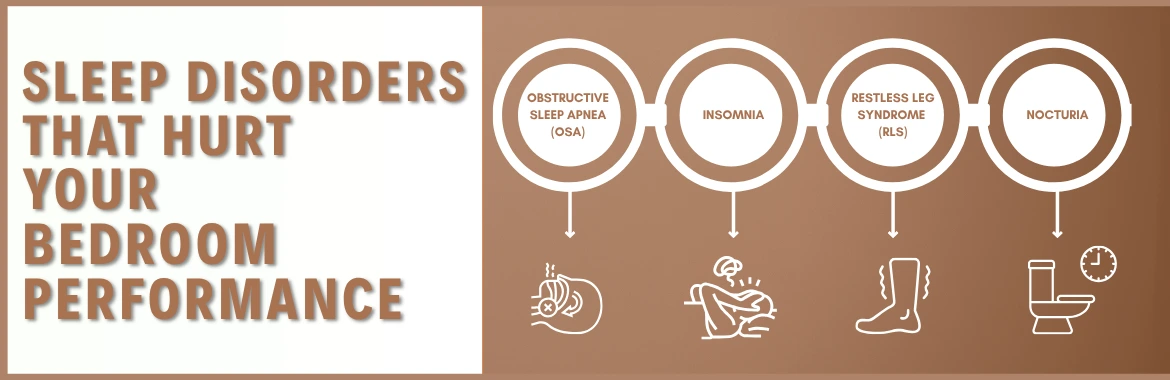
Key Sleep Disorders Contributing to ED
Not all sleep issues affect your body in the same way. Some specific disorders have a stronger link to erectile dysfunction, each with unique effects on your health.
1. Obstructive Sleep Apnea (OSA)
OSA is one of the most common sleep disorders in men. It causes repeated pauses in breathing during sleep, which lowers oxygen levels and disrupts rest. This condition is strongly linked to erectile dysfunction. Studies show that men with OSA are significantly more likely to experience ED compared to those without it.
The connection between Obstructive Sleep Apnea and ED is well-documented. Studies show ED affects between 40.9% and 80% of men with OSA. One major reason is that poor oxygen flow affects blood vessels, making it harder to get or maintain an erection. OSA also reduces the amount of deep and REM sleep, which are key for testosterone production. On top of that, men with OSA often deal with weight gain and inflammation, both of which can worsen ED.
The American Urological Association recommends checking for OSA in men with ED, especially if they snore or feel tired during the day. Treating OSA with options like Continuous Positive Airway Pressure (CPAP) therapy can lead to real improvements in sexual health.
2. Insomnia
Insomnia is when you have trouble falling asleep or staying asleep. Over time, it raises stress hormone levels and lowers testosterone. This hormonal imbalance can reduce sexual drive and make it harder to perform. Poor sleep from insomnia also affects mood, focus, and energy, all of which play a role in sexual health.
Men with chronic insomnia are more likely to report ED, even if they don’t have other health issues.
3. Restless Leg Syndrome and Nocturia
Restless Leg Syndrome (RLS) causes an urge to move the legs at night, making it difficult to stay asleep. Nocturia, or waking up multiple times to urinate, also disrupts sleep cycles. Both of these conditions can lead to fatigue and interfere with hormone balance, blood flow, and mood. While they don’t directly cause ED, the sleep loss they create can add to the problem.
What this shows is that sleep issues aren’t just about feeling tired. They can affect your body in ways that reduce sexual performance.
Whether it’s OSA, insomnia, or frequent night waking, these disorders should not be ignored when dealing with ED.
Diagnosis and Assessment of Sleep-Related Erectile Dysfunction
When erectile dysfunction shows up, it’s easy to assume it’s just stress or age. But if sleep is playing a role, identifying it early can make a big difference. That’s why a proper evaluation is key, not just for treating ED, but for improving overall health.
Diagnosing Sleep-Related Erectile Dysfunction Step What It Covers Why It Matters 1. Full History Medical & sexual background, lifestyle, stress, IIEF score Finds early ED-sleep connections 2. Key Blood Tests Testosterone, blood sugar, cholesterol, thyroid levels Detects hidden health factors 3. Sleep Screening STOP-BANG, PSQI, sleep diary Identifies risk of sleep disorders 4. Sleep Study Polysomnography or home test Confirms sleep apnea or serious sleep issues 5. Clinical Insight AUA & experts recommend sleep checks for ED Better diagnosis = better treatment *IIEF: International Index of Erectile Function
*STOP-BANG: Snoring, Tiredness, Observed apnea, high blood Pressure, BMI, Age, Neck circumference, and Gender
*PSQI: Pittsburgh Sleep Quality Index
How Better Sleep Can Boost Your Well-Being and Performance
If you’re facing any difficulties in your daily energy or focus, poor sleep might be a bigger factor than you realize. The good news? Improving your sleep can make a significant difference in how you feel and function every day.
1. Tackling Hidden Sleep Problems First
For example, if sleep apnea is a concern, using a CPAP machine often helps. This device keeps your airway open during sleep, improving oxygen levels and hormone balance.
Better breathing at night often leads to better days.
In some cases, surgery or special oral devices might be necessary depending on individual needs. If insomnia is the problem, treatments like cognitive-behavioral therapy (CBT) and adopting good sleep habits can be very effective.2. Small Lifestyle Tweaks That Make a Big Difference
Lifestyle changes also play a huge role in improving sleep quality and overall health. So one should:
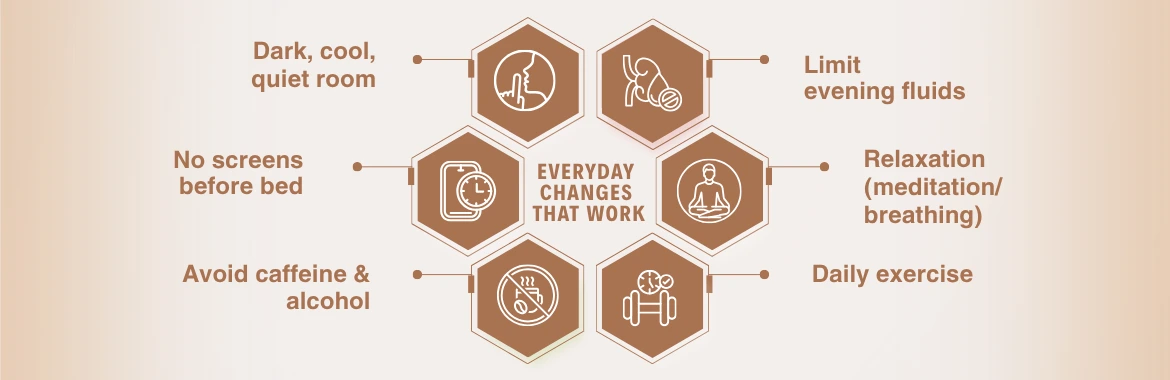
3. Don’t Overlook Other Health Factors
Losing excess weight can improve breathing and hormone levels. Managing blood sugar and blood pressure is also essential for maintaining good circulation and energy.
If you’ve tried all these tips and still have trouble sleeping or other symptoms, consulting a healthcare professional can help you get personalized advice and treatment.
Important Note: In some cases, doctors may recommend erectile dysfunction medications to help improve blood flow and support erections. These can be effective, but it’s important to address any underlying sleep problems at the same time to get the best results
Conclusion
As a wrap-up, you now understand why prioritizing sleep is crucial to feeling your best in bed.
Making sleep a priority is not just about avoiding tiredness. It’s about supporting your overall health and improving your quality of life in ways you might not expect.
So, before you sacrifice sleep, remember this: Good sleep could be the key to unlocking your full potential.
Disclaimer: This content is for informational purposes only and is not a substitute for medical advice. Always consult a healthcare provider for diagnosis or treatment.