What does it mean to be young? Most of you would say it’s about being energetic, healthy, and full of life. You see young men hitting the gym, running outdoors, and doing everything to stay in shape. And yet, for many of you, something feels off, especially during intimate moments.
You’re young, you take care of your body, and still, things aren’t clicking when it matters most. At first, you might dismiss it. Maybe it’s stress, you tell yourself. But when it happens more than once, frustration and confusion set in. Sound familiar?
You’re not alone. More and more young men today are facing erectile dysfunction (ED). And no, it’s not just an “older man’s issue” anymore.
Here’s the part no one talks about enough: ED in young men is on the rise, and it’s time to start having honest conversations about it without shame or stigma.
In this blog, you’re going to explore the facts, clear up the confusion, and answer the big questions:
-
- Is ED common in young men?
- What causes it?
- And more importantly, what can you do about it?
Let’s start by breaking down what ED really is and why it’s no longer just a concern for men over 40.
Demystifying Erectile Dysfunction in Younger Men
You might hear the term erectile dysfunction all the time, but what does it really mean?
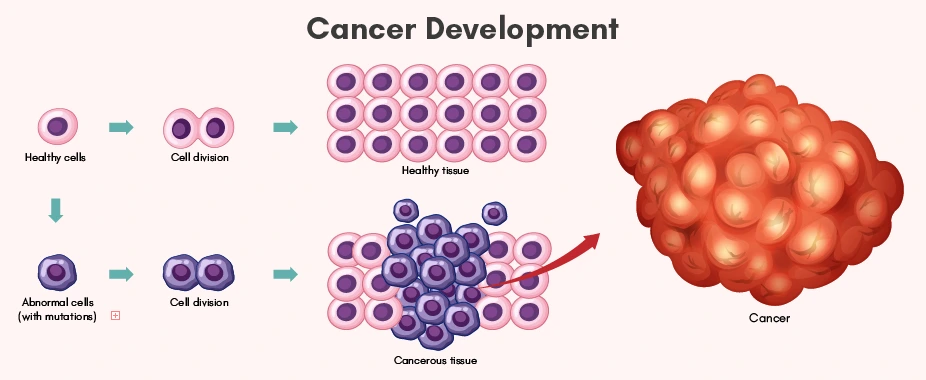
Simply put, ED is when a man can’t get or keep an erection firm enough for sex consistently. An occasional off-night is normal. But if it keeps happening, it can affect more than just your intimate life. It can impact your confidence, relationships, and mental health, and sometimes signal deeper health problems.What Happens in the Body?
Getting an erection isn’t just about being in the mood. It’s actually a complex process involving:
- Your brain (mental stimulation)
- Hormones like testosterone
- Nerves that signal the muscles
- Blood vessels that carry blood to the penile area
- And even your heart, which keeps everything circulating
If any part of this system is out of sync, things may not work as expected. And for many young men, there can be multiple small disruptions adding up over time.
Why is ED Common in Young Men?
In the past, ED used to be thought of as an “older man’s issue.” But recent research shows that this is no longer true. Erectile Dysfunction in the 20s is very common. Here’s what the numbers say, as per different sources:

As you can see, ED in young men isn’t rare anymore—it’s alarmingly common.
“Wait… Is This that Normal?” So, Why Is It So Hard to Talk About
Despite the rising numbers, many young men feel like they’re the only ones going through this.
Why? Because of the stigma.
There’s a deep-rooted belief that ED is something older men deal with. So when it happens to someone in their 20s or 30s, it often leads to:
- Embarrassment
- Delays in seeking help
- Self-blame
- And sometimes, avoiding intimacy altogether
But here’s what’s even more concerning: studies show that when young men do go to the doctor for ED, they’re more likely to be facing severe forms of it compared to older men.
That’s a huge red flag and a clear reason why early awareness and treatment are so important.
Let’s uncover what’s really behind the rise of ED in younger guys.What Causes Erectile Dysfunction in Younger Men?
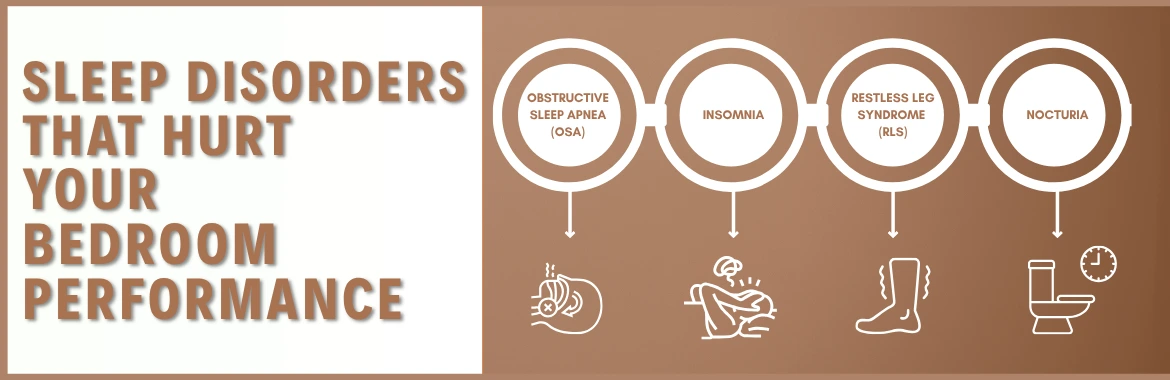
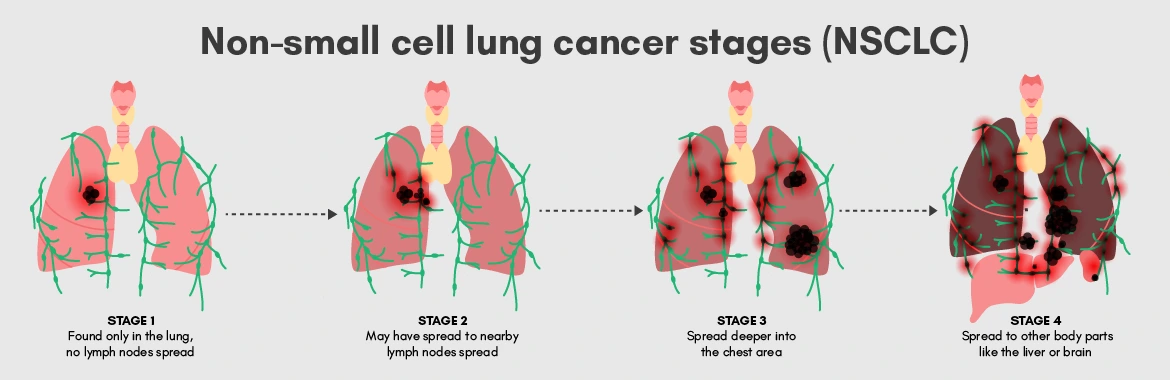
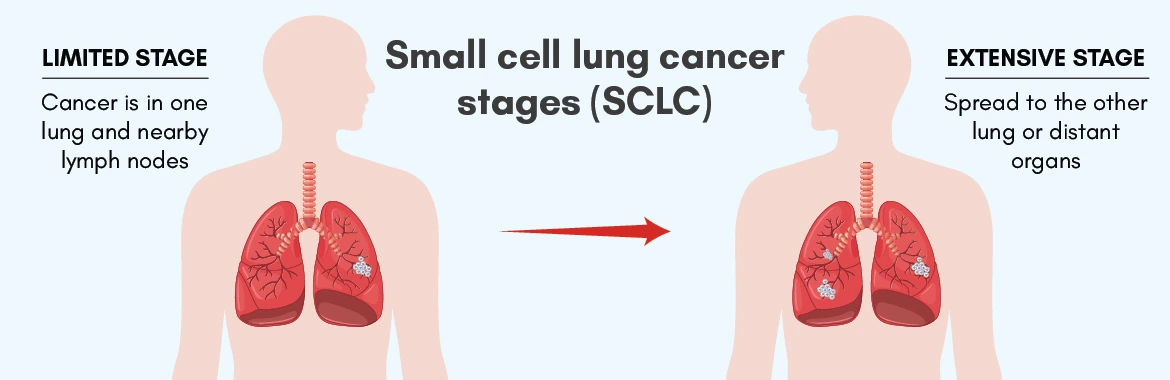
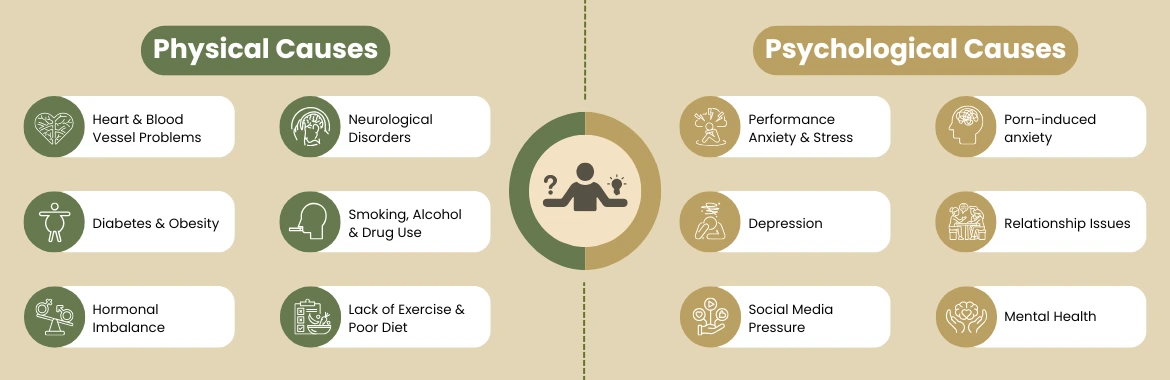
Erectile dysfunction in younger men is usually caused by a mix of mental, physical, and lifestyle factors. While psychological issues were once seen as the main cause, studies now show that organic (physical) causes are just as common. Let’s break down the causes of ED in younger men:
Getting the Right Diagnosis: What Happens When You See a Doctor for ED
If you’re a younger guy facing erectile dysfunction (ED), a proper check-up is crucial. It helps identify the cause and catch serious health issues like heart problems or diabetes early. While discussing ED can feel awkward, doctors are aware and ready to help. Opening up is the first step to improvement.
Here’s what usually happens during the evaluation:
- Health History: Overview of health, medications, and family history.
- Sexual History: Start of symptoms, severity, and natural erections during sleep or masturbation.
- Stress and Emotions: Screening for anxiety, depression, and relationship issues.
- Physical Exam: Assessing physical signs, nerve function, and hormone changes.
- Lab Tests: Blood and urine tests for diabetes, cholesterol, testosterone, etc.
- Special Tests: May include blood flow ultrasounds or overnight erection tests.
- Mental Health Evaluation: Assessing the impact of stress or anxiety.
One should know when to seek medical help for ED before it’s too late.List of Treatment Approaches For Younger Men with ED
Dealing with ED can feel overwhelming, especially when you’re young, and it hits unexpectedly. The good news? There are plenty of ways to tackle it, and many don’t start with medication right away.
First things first: Treatment depends on what’s causing your ED. A balanced approach that considers the whole picture tends to work best.
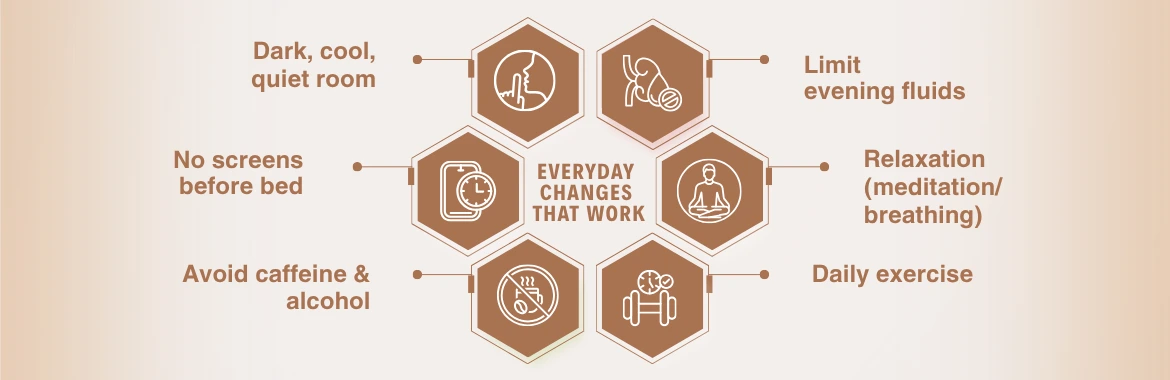
1. Lifestyle Tweaks That Make a Real Difference
Believe it or not, small changes can pay off big time. Think of these as the groundwork before jumping into meds:
- Eat healthy, focus on fruits and veggies.
- Exercise regularly for better blood flow.
- Manage stress through relaxation techniques.
- Avoid smoking and heavy drinking.
- Get enough sleep for hormone balance.
- Communicate openly with your partner.
If stress or relationship troubles play a part, therapy or counseling can be a game-changer. It’s not just “in your head,” it’s real help for real issues.
Check this page to learn about diet and nutrition for erectile dysfunction, which includes what to eat (and what to avoid).
2. Medications — Your Go-To Tools
When lifestyle changes aren’t enough, doctors often recommend meds belonging to the class of PDE5 inhibitors. These are the most common and trusted drugs for ED.
Here’s the quick rundown:
- Sildenafil: Works for 4-6 hours. Take it about an hour before sex.
- Tadalafil: Stays active up to 36 hours, which means more freedom to be spontaneous.
- Vardenafil: Fast-acting and similar to sildenafil.
- Avanafil: Known for working quickly with fewer side effects for some guys.
These meds relax the blood vessels in your penile area, helping blood flow in the penile region when you’re aroused. Looks easy, right?
But a few important notes:
- They don’t cause erections on their own; you still need sexual stimulation.
- Side effects can include headaches, flushing, or upset stomach.
- Never mix these meds with nitrates (heart meds); that combo can dangerously lower your blood pressure.
- Don’t use them just for fun or without a doctor’s okay. Misusing these drugs can backfire badly.
3. Other Medical Options
If pills aren’t effective, there are other options available, but only with a doctor’s prescription:
-
- Injectables like Alprostadil can be injected into the genital area for a quick erection when pills aren’t effective.
- Urethral suppositories are another alternative that involves placing tiny meds inside the penile region.
Both can cause some discomfort or rare side effects like a prolonged erection that needs urgent care. So, you’ll want to be properly guided.
- Vacuum erection devices use suction to draw blood into the penile area and maintain an erection with a ring. They are non-drug and non-surgical but may feel somewhat awkward.
- Hormone therapy can boost libido and erections if low testosterone is the issue, but it requires medical supervision and is for specific cases only.
4. When Surgery is the Answer
Doctors usually recommend surgery as the last stop, only when all other treatments have failed or in cases of severe damage due to injury or disease. The options for surgery include:
- Penile implants
- Penile vascular surgery
DID YOU KNOW?…
New and exciting treatments for ED are currently being researched. There’s some buzz around shockwave therapy and platelet-rich plasma, but these are still being studied and aren’t routine yet. They offer hope, especially for those wanting to avoid meds or surgery.
Wrapping It Up
Remember how we talked about how ED isn’t just about physical issues but also stress, lifestyle, and even your mindset? Well, that’s why tackling it means looking at the whole picture, not just popping a pill.
If you’re a younger guy experiencing ED, don’t feel ashamed, it’s common and doesn’t define you. Think of it as a signal to check for possible underlying health issues.
Be open about it: talk to your doctor, share with your partner, and focus on healthy habits like sleep, exercise, and stress management. If medication is needed, use it wisely.
Your sexual health is tied to your overall well-being, so taking action now can boost your confidence and relationships. Take that first step and own it!
Disclaimer: This content is intended for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment of medical conditions.