Hormones play a crucial role in regulating various bodily functions, including metabolism, mood, growth, and reproductive health. While both men and women can experience hormonal imbalances, women are particularly susceptible due to distinct hormonal cycles such as menstruation, pregnancy, and menopause. Understanding hormonal imbalances is crucial for maintaining good health and overall well-being.
What is Hormonal Imbalance?
When the body produces either too many or too few hormones compared to optimal physiological levels, this is known as a hormonal imbalance. Hormone imbalances can lead to various health issues because they are crucial for numerous bodily processes.
Key Hormones That Affect Women
- Estrogen: The development and control of the female reproductive system, as well as secondary sex traits, depend on this major female hormone. A woman’s health is significantly influenced by her estrogen levels, which fluctuate throughout the menstrual cycle.
- Progesterone: This hormone prepares the woman’s body for pregnancy each month and maintains the early stages of pregnancy. If pregnancy doesn’t occur, progesterone levels drop, leading to menstruation.
- Testosterone: This hormone is often known as a male hormone, but it is also crucial for women. Though produced in lower quantities, it plays a vital role in energy, libido, and mood stability.
- Hormones: These hormones, produced by the thyroid gland, regulate energy levels, heart rate, and metabolism. Conditions like hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid) can be brought on by imbalances and cause a variety of symptoms.In simple terms, a hormonal imbalance is like a symphony gone off-key. When one hormone overpowers or fades out, the whole body feels out of tune.
Causes of Hormonal Imbalance in Women
A range of factors can contribute to hormonal imbalances in women. Understanding these causes is essential for prevention and treatment:
1. Lifestyle Factors
- Poor Diet: A high intake of processed sugars and unhealthy fats can lead to insulin resistance, which may result in hormonal imbalance. Insulin resistance occurs when the body becomes less responsive to insulin, leading to increased levels of male hormones (androgens). Conversely, a diet rich in whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, supports hormonal health and can help regulate hormone production.
- Lack of Exercise: Sedentary lifestyles are associated with numerous health problems, including obesity, which can have a detrimental effect on hormone levels. Maintaining a healthy weight, lowering stress levels, and encouraging the production of hormones that improve mood and well-being all depend on regular physical activity. Every week, aim to incorporate at least 150 minutes of moderate aerobic activity, along with weight training.
- Chronic Stress: When subjected to prolonged stress, the body produces elevated levels of cortisol, commonly referred to as the stress hormone. High cortisol levels can disrupt other hormone functions, resulting in symptoms such as mood swings, weight gain, and fatigue. Incorporating stress-relief techniques, such as yoga, meditation, or engaging in enjoyable hobbies, can help lower cortisol levels and improve overall hormonal balance.
2. Medical Conditions
- Polycystic Ovary Syndrome (PCOS): One of the most prevalent hormonal conditions affecting women who are of reproductive age is PCOS. Ovarian cysts, excessive hair growth (hirsutism), and irregular menstrual periods are its hallmarks. A disturbed hormonal balance results in women with PCOS frequently having high levels of androgens, or male hormones. Acne, weight gain, and thinning of the scalp hair are additional common signs.
- Thyroid Disorders: Disorders of the thyroid gland may lead to significant hormonal imbalances. Underactive thyroid or hypothyroidism may lead to symptoms of tiredness, weight gain, and depression, whereas overactive thyroid or hyperthyroidism may lead to anxiety, weight loss, and rapid heart rate. Both of these may disrupt the usual production of thyroid hormones and have a great impact on one’s health.
- Diabetes: Conditions like Type 2 diabetes are closely linked to hormonal imbalances, particularly those related to insulin. Insulin, a hormone responsible for regulating blood sugar levels, can become imbalanced due to insulin resistance. Since insulin is a hormone, imbalances in insulin levels can disrupt the broader endocrine system. This disruption can have a cascading effect on other hormones, leading to additional health complications if not managed effectively. Other causes may include adrenal disorders like Cushing’s syndrome or Addison’s disease, which affect cortisol levels.
3. Age-Related Changes
- Menopause: A woman’s reproductive years come to an end at this point, typically occurring between the ages of 45 and 55. The natural decrease in estrogen and progesterone levels that occurs during menopause causes a number of symptoms, such as mood swings, hot flashes, sleep issues, and weight gain. Some women may experience severe symptoms that drastically affect their quality of life.
- Perimenopause: The transitional phase leading to menopause is referred to as perimenopause, during which hormone levels fluctuate significantly. Women may notice changes in their menstrual cycles, increased mood swings, and other emotional or physical symptoms well before reaching menopause.
- Age-related changes, medical issues, and lifestyle choices can all contribute to hormonal imbalances. Women can take proactive measures to manage their hormonal health by being aware of these aspects.
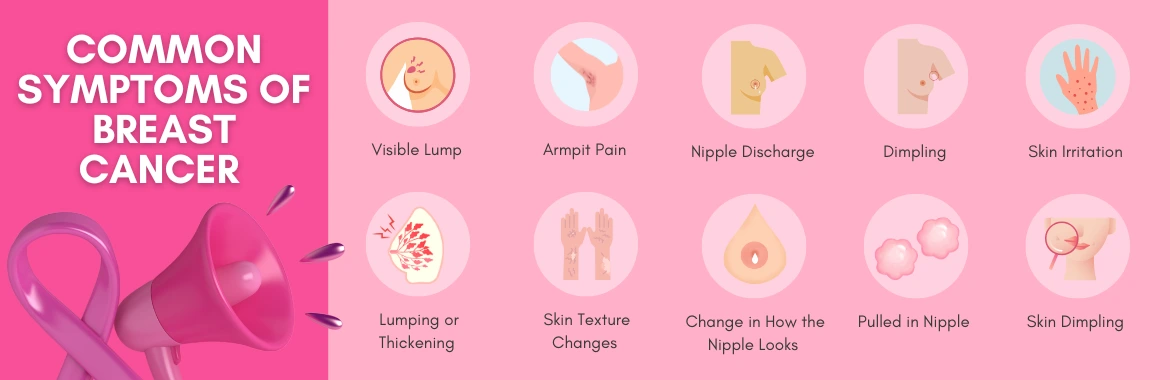
Symptoms of Hormonal Imbalance
Identifying hormonal imbalance symptoms is crucial for obtaining timely medical treatment. The symptoms of hormonal imbalance differ widely among individuals and may include a variety of physical and emotional signs.
Common Symptoms
1. Physical Symptoms:
- Irregular Periods: Having menstrual cycles that are too long, too short, or inconsistent can indicate a hormonal imbalance.
- Weight Changes: Sudden weight gain or loss without any changes in eating habits or activity level can be a red flag.
- Fatigue: Constant tiredness that does not improve with adequate sleep may suggest hormonal issues.
- Acne or Oily Skin: Inconsistent hormone levels can lead to increased oily skin and breakouts, particularly in adulthood.
2. Emotional Symptoms:
- Mood Swings: Wide-ranging emotional fluctuations, irritability, and anxiety can be linked to hormonal changes.
- Low Libido: A noticeable drop in sexual desire may be attributed to imbalances in estrogen or testosterone.
Specific Symptoms by Hormone Imbalance:
| Hormone | Role | Imbalance Effects |
| Estrogen | Regulates the menstrual cycle, bones | Hot flashes, irregular periods |
| Progesterone | Supports pregnancy, sleep | PMS, insomnia, anxiety |
| Testosterone | Boosts libido, energy, and muscle | Fatigue, mood shifts |
| Thyroid | Controls metabolism | Weight gain/loss, hair thinning |
There are many different ways that hormonal abnormalities can show up; knowing these signs can help women decide whether to get help from a doctor.

Treatment Options for Hormonal Imbalance
There are various treatment methods available once a hormonal imbalance is detected. The most effective treatment typically depends on the specific hormones affected, the underlying causes of the imbalance, and individual health needs. The following are some major treatment strategies to take into account:
A. Lifestyle Changes
Typically, the first line of treatment for hormone imbalances involves making healthy lifestyle modifications. Here are some easy-to-incorporate lifestyle changes:
- Balanced Diet: A well-rounded, nutrient-rich diet can have a significant impact on hormonal health. Here’s how to construct a diet that promotes balance.
- Whole Foods: Focus on consuming unprocessed foods that are high in nutrients. Incorporate plenty of fruits and vegetables, which provide essential vitamins, minerals, and antioxidants that support hormonal function.
- Healthy Fats: Include sources of omega-3 fatty acids, such as fatty fish (salmon, mackerel), flaxseeds, walnuts, and chia seeds. These fats can help reduce inflammation and may assist in hormone production and regulation.
- Lean Proteins: Include lean proteins like chicken, turkey, and legumes. Protein is needed for hormone production and various bodily functions.
- Fiber-Rich Foods: High-fiber foods, such as whole grains, legumes, fruits, and vegetables, can help regulate blood sugar levels and enhance insulin sensitivity, which is crucial for maintaining hormonal balance.
- Hydration: Staying well-hydrated is crucial for overall health and can help maintain hormonal levels. Aim to drink an adequate amount of water throughout the day, as dehydration can impact energy levels and mood.
- Phytoestrogen-rich diet: Include phytoestrogen-rich foods like flaxseeds, soy, and sesame, which may help balance estrogen levels naturally.
B. Regular Exercise Routine
Both excessive and insufficient exercise can disrupt cortisol and estrogen levels, which is why physical activity is a powerful tool for managing hormonal balance:
- Types of Exercise: Engage in a combination of aerobic exercises (such as walking, running, and cycling) and strength training (like weight lifting or resistance band exercises). This combination promotes both cardiovascular health and muscle strength, which are critical for hormonal regulation.
- Regularity: Aim for at least 150 minutes of moderate exercise per week. Regular physical activity can reduce stress, improve mood, and enhance overall hormonal health.
- Mind-Body Exercises: Incorporating practices like yoga or Pilates can help lower stress levels and promote hormonal balance by providing relaxation, enhancing flexibility, and improving physical strength.
C. Stress Management Techniques
Chronic stress triggers the HPA axis, leading to overproduction of cortisol, which can suppress reproductive hormones like estrogen and progesterone, so it’s essential to integrate effective stress management strategies into your routine:
- Mindfulness and Meditation: Mindfulness, or the practice of meditation, can also be a highly effective method for lowering cortisol levels. A few minutes every day can make an impressive difference in one’s state of mind.
- Deep-Breathing Exercises: Engaging in deep-breathing exercises can trigger the body’s relaxation response, helping to soothe the nervous system and reduce stress.
- Engaging in Hobbies: Spend time doing things you enjoy, whether it’s reading, gardening, or painting. Joyful activities can be great stress relievers.
2. Hormone Replacement Therapy (HRT)
Some women, especially those who have severe symptoms at menopause, might find hormone replacement therapy (HRT) to be appropriate. HRT is a prescribed medication that includes estrogen, progesterone, or both to alleviate symptoms resulting from hormone changes. HRT is available in forms such as pills, patches, creams, and pellets, which are selected based on symptom severity and individual health profiles.
Benefits of HRT:
- Symptom Relief: Hot flashes, nocturnal sweats, and mood swings are just a few of the menopausal symptoms that HRT can significantly reduce.
- Bone Health: HRT may help protect against osteoporosis, a condition where bones become weak and brittle.
- Improved Quality of Life: Many women report an enhanced overall quality of life while undergoing hormone replacement therapy (HRT).
Risks and Considerations:
- Health Risks: Some research has shown possible dangers linked to HRT, such as enhanced risk for certain cancers, blood clots, and cardiovascular issues. A comprehensive consultation with a medical professional is essential to balance the risks and benefits.
- Individualized Approach: The decision to begin HRT should be personalized, taking into account family history, symptom severity, and individual health profiles.
3. Natural Remedies
While Hormone Replacement Therapy (HRT) offers significant benefits for managing hormonal imbalances, it’s essential to be aware of potential risks. It is necessary to understand that while some herbal remedies show promise, they are not FDA-approved for treating hormonal imbalances. Consult your healthcare provider before use. These natural solutions can be incredibly helpful in gently balancing your hormones.
| Natural Remedy | Potential Benefits |
| Vitex (Chaste Tree) | Regulates menstrual cycles, alleviates PMS symptoms |
| Black Cohosh | Eases menopause symptoms, like hot flashes |
| Maca Root | Boosts energy, balances hormones |
| Vitamin D | Regulates hormones, supports mood |
| Omega-3 Fatty Acids | Reduces inflammation, enhances hormonal balance |
| Magnesium | Supports hormone production, reduces anxiety |
| Ashwagandha and Rhodiola | They are adaptogens, which are shown to reduce cortisol and improve hormonal resilience under stress. |

Daily Hormone Balancing Checklist: Proactive Steps for Balance
Prevention is often the best treatment. Use this checklist to incorporate healthy habits into your routine and support your hormonal well-being. Tick them off as you go!
1. Nourish Your Body (Diet)
- Incorporate Whole Foods:
- Aim for a balanced plate with lean proteins, healthy fats, and a colorful array of fruits and vegetables at every meal.
- Reduce Processed Sugars and Refined Carbohydrates:
- Limit sugary drinks, sweets, and highly processed snacks.
- Choose whole grains over refined grains (e.g., brown rice instead of white rice, whole wheat bread).
2. Move Your Body (Exercise)
- Aim for At Least 30 Minutes of Moderate Exercise Daily:
- Find an activity you enjoy, such as brisk walking, swimming, cycling, dancing, or yoga. Consistency is key!
3. Calm Your Mind (Stress Management)
- Engage in Relaxation Activities Regularly:
- Practice mindfulness or meditation for a few minutes each day.
- Incorporate breathing exercises into your routine.
- Dedicate time for self-care activities that help you unwind (e.g., reading, a warm bath, spending time in nature).
4. Stay Informed (Regular Check-Ups)
- Consult with Healthcare Providers:
- Schedule regular check-ups, especially if you notice symptoms of hormonal imbalance.
- Discuss any concerns with your doctor to ensure early detection and intervention.
Conclusion
Hormonal imbalances can have a substantial impact on women’s health, affecting everything from physical welfare to mental stability. Understanding your hormones is the first step. Whether through lifestyle changes, hormone replacement therapy (HRT), or holistic care, you can find your balance. Don’t ignore the signals—talk to a healthcare provider and take charge of your hormonal health today. Taking charge of your hormonal health is a crucial first step toward overall well-being, and you can effectively navigate the challenges of hormonal balance if you are proactive and informed.